
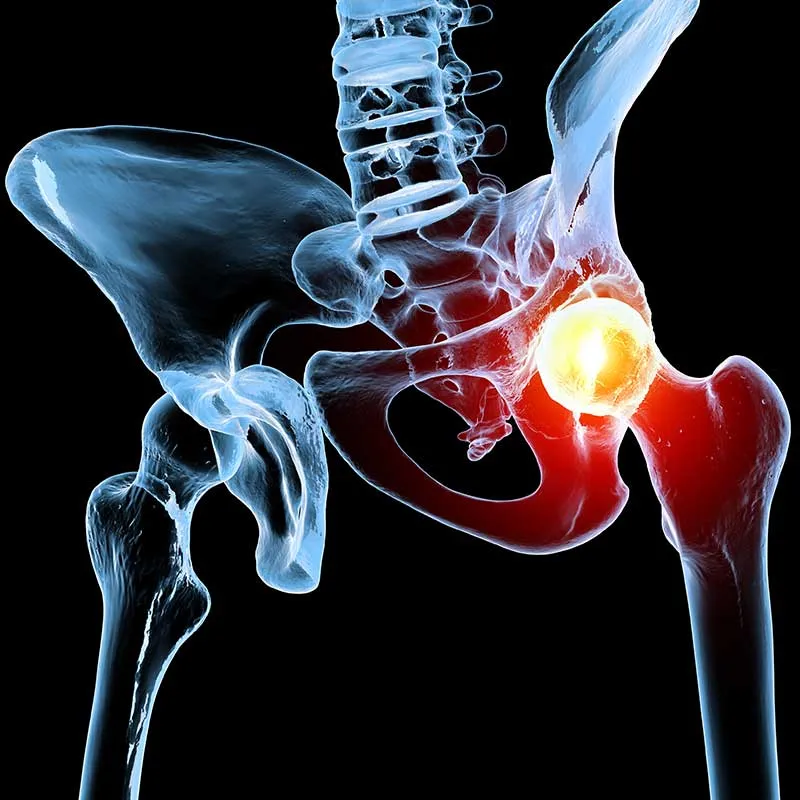
Hip osteoarthritis describes a process of degenerative change within the hip joint. It is a common condition that affects the cartilage, that cushions and protects the ends of bones in the hip joint. Over time, the cartilage in the hip joint can undergo degenerative change, resulting in wear and thinning, leading to pain, stiffness, inflammation and loss of function in the hip.
Contact Us 020 8004 6659Hip osteoarthritis is most common in adults over the age of 50, with risk increasing with age. Women are more likely than men to develop hip osteoarthritis, especially after menopause. Other factors that increase the risk of hip osteoarthritis include:

Excess weight puts extra stress on the hip joint.

Injuries to the hip, such as fractures or dislocations, can increase the risk of developing osteoarthritis later in life.
Having a family history of osteoarthritis increases your risk of developing it yourself.

Jobs that require repetitive hip movements or heavy lifting can increase the risk of developing hip osteoarthritis.
The main symptoms of hip osteoarthritis include:

Symptoms may worsen gradually over time and may fluctuate depending on the level of activity. Activities that involve weight-bearing, such as walking, climbing stairs, or standing for long periods, tend to aggravate the pain and discomfort.

Diagnosis of hip osteoarthritis typically involves a physical examination, medical history review, and imaging tests.
Treatment for hip osteoarthritis focuses on managing symptoms, slowing the progression of the condition, and improving function. Non-surgical treatments are usually tried first, and surgery is considered if non-surgical measures fail to provide adequate relief.


Corticosteroid injections can be an effective way of reducing inflammation and pain in the hip joint. At The Joint Injection Clinic, corticosteroid injections are performed after a thorough consent process, whereby the risk and benefits of the procedure are discussed in detail with your doctor. The experienced medical doctor will then place you in a lying position with the front of the hip facing upwards. The skin is cleaned using a cleaning solution to ensure that the procedure is performed under sterile conditions. Local anaesthetic is injected from the skin to the joint under ultrasound guidance. After giving the local anaesthetic a few minutes to take effect, the hip joint injection is performed with a small dose of steroid and local anaesthetic, targeting the front part of the ball and socket joint.
The injection itself is normally completed within 30-60 seconds, after which a plaster is applied and post-injection advice is given. The patient is advised to look out for any signs of infection, specifically to check whether the local area becomes red, hot, tender, swollen or if they develop a fever. If this occurs then the patient is asked to contact the clinic immediately at which time a formal reassessment will occur and if needed oral antibiotics can be prescribed. The patient is also warned that following any injection they may notice a short-term worsening or flare in their symptoms after the local anaesthetic has worn off (4-5 hours). This may last for 3-5 days and the patient is advised to consider icing of the area using an ice pack for 10-15 minutes every hour as required.

If non-surgical treatments fail to provide adequate relief, surgery may be considered. Surgical options for hip osteoarthritis include:
Surgery is typically considered for patients with severe hip osteoarthritis that causes severe pain or significantly impacts their quality of life and limits their ability to perform daily activities.
Additional tips for managing hip osteoarthritis pain: