
First carpometacarpal joint (1st CMCJ) osteoarthritis, also known as base of thumb arthritis is a degenerative condition that affects the joint at the base of the thumb, where the trapezium bone meets the first metacarpal bone. This joint is important for thumb movement and plays a role in gripping, pinching, and lifting of the thumb.
1st CMCJ osteoarthritis is more prevalent in women than men, with the incidence increasing significantly after the age of 50. It is estimated that up to 25% of women aged 75 years and older may experience this condition.
Risk factors for developing 1st CMCJ osteoarthritis include:

The primary symptoms of 1st CMCJ osteoarthritis include:

Pain at the base of the thumb, often described as a sharp or aching sensation that worsens with thumb movement and may radiate into the palmar side of the thumb or into the back of the thumb, into the area between the thumb and index finger.

Limited range of motion in the thumb, making it difficult to perform tasks like grasping, pinching, or rotating the thumb, i.e. turning a key to open a lock

Swelling around the base of the thumb, which may be visible or palpable.

Increased sensitivity to touch at the base of the thumb.

Reduced grip strength and difficulty holding objects.

Crepitus, or grating or clicking sounds, when moving the thumb.
Symptoms tend to worsen gradually over time and may fluctuate in severity. Activities that involve thumb movements, such as typing, gripping objects, or turning doorknobs, can exacerbate pain and discomfort.
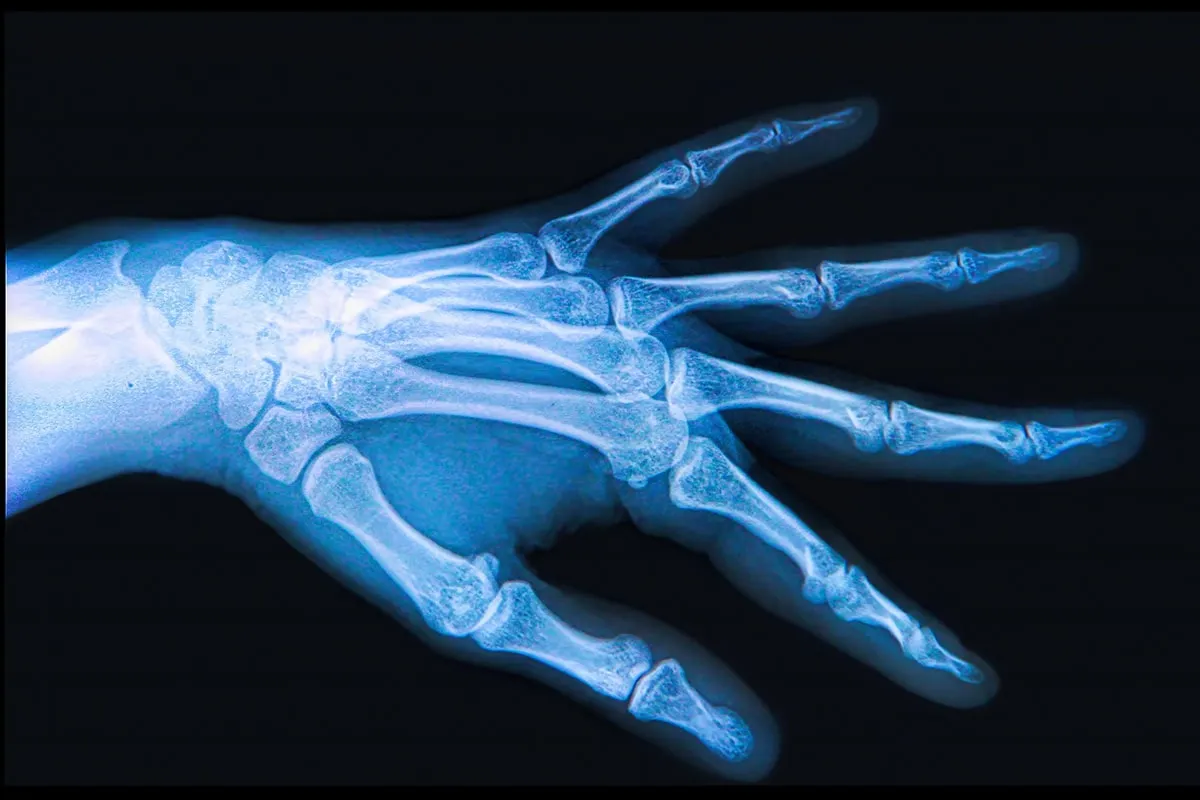
Diagnosis of 1st CMCJ osteoarthritis typically involves a thorough medical history, physical examination, and imaging tests.
Treatment for 1st CMCJ osteoarthritis focuses on managing symptoms, improving function, and slowing the progression of the condition. Non-surgical treatments are usually tried first, and surgery is considered if non-surgical measures fail to provide adequate relief.


At The Joint Injection Clinic, these injections are performed after a thorough consent process, whereby the risk and benefits of the procedure are discussed in detail with your doctor. The experienced medical doctor will then place you in a seated position with your hand resting on the couch. The hand is cleaned using a cleaning solution to ensure that the procedure is performed under sterile conditions. The combined local anaesthetic and steroid is injected from the skin to the joint under ultrasound guidance.
The injection itself is normally completed within 30 seconds, after which a plaster is applied and post-injection advice is given. The patient is advised to look out for any signs of infection, specifically to check whether the local area becomes red, hot, tender, swollen or if they develop a fever. If this occurs then the patient is asked to contact the clinic immediately at which time a formal reassessment will occur and if needed oral antibiotics can be prescribed. The patient is also warned that following this particular injection they may notice a short-term worsening or flare in their symptoms after the local anaesthetic has worn off (4-5 hours). This may last for 3-5 days and the patient is advised to consider icing of the area using an ice pack for 10-15 minutes every hour as required.
The best treatment option for you will depend on the severity of your 1st CMCJ arthritis, your overall health, and your activity level.
If you are experiencing pain and stiffness in your thumb, it is important to see a doctor to get a diagnosis and discuss treatment options.